Acute Coronary Syndrome Algorithm Video
Hi. I’m Mark for ACLS Certification Institute. Welcome back to another Rapid Algorithm Review. Today we’re going to cover ACS (acute coronary syndrome). It all starts with the patient, the patient’s presentation. When we think about heart attacks and acute coronary syndrome, we tend to think of the typical symptoms: chest pain, shortness of breath, pain radiating up into the shoulder, maybe up into the jaw. Remember that in women an unusual fatigue by itself can be a symptom of a heart attack and should be suspect for acute coronary syndrome, so in women an unusual fatigue. In men, remember that if a patient wanted to, they could fake any symptom. They could fake the chest pain. They go, “Oh, my chest hurts. I’m having trouble breathing. My butt itches.” They can fake every symptom they want except sweating. A patient cannot fake diaphoresis. If you show up at the scene or you have a patient come into your emergency room, they have shortness of breath, are complaining of chest tightness and are sweaty, they’re in trouble. Everybody’s in trouble, and it’s time to go to work. Remember, it starts with the patient’s presentation.
You’ve determined your patient is having an acute coronary event. Time to go to work. Looking at the algorithm, there are all these different things we need to do. In reality, these are going to happen in concert. Somebody’s calling the shots. We tend to do all these at the same time. Support the ABCs if needed and be prepared for things to go south. We have an ischemic heart that can become irritated very easily, so have your defibrillator and resuscitative gear ready. We’re going to oxygenate to achieve an SPO2 of 94% to 95%. We need to get this patient on a monitor, get an IV in them, get a 12-lead EKG, start administering our medications. If there’s no contraindication, aspirin administration and nitroglycerin, again, if there’s no contraindication.
You can ask the guy, “Sir, have you taken Viagra or Cialis within the last 24 to 48 hours?” He may look at you and go, “No, I’m like a Turkish soldier once served at a circus freak show.” Then you say, “Okay, sir, that’s fine, but if you’re taking that drug and I give you this drug, it may potentiate it and cause a precipitous fatal drop in your blood pressure and we may not even make it to the parking lot.” Then he goes, “Oh, Viagra. I thought you asked if I had a Snickers bar. Yes, I have had Viagra within the last 24 hours.”
Do not administer the nitro. Again, it can cause a precipitous fatal drop in their blood pressure. Get that 12-lead EKG. Remember, we’re looking for ST-segment elevation. If your patient’s having ST-segment elevation, notify the receiving facility immediately, so they can prepare to receive this patient and get things moving so we can open up that coronary vessel when they hit the door.
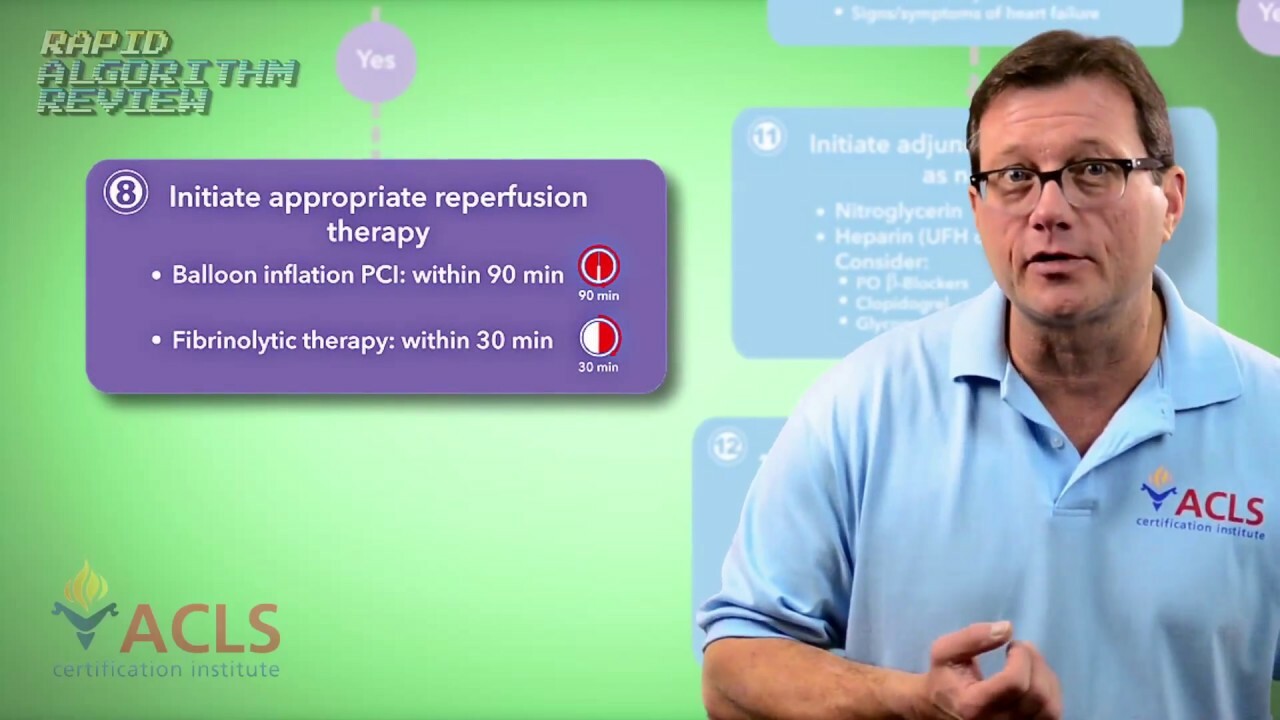
If you’re in the emergency department and you’re receiving a patient from the field, a code STEMI, within the first 10 minutes of their arrival, we want to do a few things. First, reassess the patient. Get an updated set of vital signs, review their history, ensure adequate oxygenation, ensure adequate vascular access. We want to try to get a chest x-ray within the first 30 minutes, but if that’s part of your code STEMI response, x-ray should already be at the door when they hit the door. Administer your medications if they haven’t already been administered—your aspirin and your nitro if there is no contraindication. Retake a 12-lead EKG. Again, we’re looking for ST-segment elevation. If that 12-lead is showing ST-segment elevation or a new or presumed left bundle branch block, game’s on. Time to open up that coronary vessel. The patient’s either going right to the cath lab or, because we’ve already started our fibrinolytic checklist, they may receive tPA right there in the ER.
Looking at the algorithm, there are a couple of suggested timeframes for opening up this vessel. If we’re using fibrinolytic therapy, it should be within 30 minutes. That’s our goal. We should have done our exclusion checklist within the first 10 minutes of the patient hitting the ER. If they’re going to the cath lab, door-to-balloon-up time within 90 minutes. That’s our goal. That’s why it’s so important in the field to call early. Give the hospital time to prepare to receive this patient. Get everything in line so we can reduce the time it takes us to open up that vessel and reperfuse the heart.
If your 12-lead doesn’t show ST-segment elevation but instead some depression or T-wave inversion, which could mean ischemia, and your patient is still having complaints consistent with an AMI, you still may want to follow your protocol, still consider your nitro and your aspirin therapy, and get an expert involved in this patient right away. Other medications to consider: heparin, IIb/IIIa inhibitors, and beta-blockers. Remember, beta-blockers are going to help slow the heart rate down and reduce the force of contractility, thus reducing the heart’s oxygen requirements. It’s kind of like an engine with a gummed up fuel line; the beta-blockers are taking your foot off the gas.
Your 12-lead shows no ST-segment elevation, no T-wave inversion, and you have a normal 12-lead, but your patient still has complaints. We’re not going to let them walk out of the ER just yet. Maybe run some labs, look at your cardiac markers, and then watch for changes in that patient’s condition. The 12-lead was normal and labs came back normal. We’re getting ready to discharge this patient, but discharge them with the instructions that should any of these symptoms recur, immediately call 911.
I’m Mark for ACLS Certification Institute. This has been Rapid Algorithm Review for acute coronary syndrome. Remember, like us on Facebook and, please, become a subscriber to our YouTube channel. Thanks, and see you in the next video.