Hypokalemia and Hyperkalemia
Potassium Homeostasis
Potassium blood level is dependent on the association between dietary potassium intake, the distribution of potassium between the cells and extracellular fluid, and urinary potassium excretion.1 Potassium secretion is dictated by an increase in the serum potassium concentration, a rise in plasma aldosterone concentration, and enhanced delivery of sodium and water to the distal secretory site.1 All of these factors contribute to potassium homeostasis- a disruption of one property will cause hypokalemia or hyperkalemia.
What is hypokalemia?
The normal dietary intake of potassium is 40 to 120 milliequivalents per day; most of this potassium is excreted in the urine. A function of the kidney is to regulate blood levels of potassium to maintain homeostasis. In the event of poor potassium intake, the kidney can lower potassium excretion to about 5 to 25 milliequivalents, thus maintaining a baseline serum potassium level of 3.5 milliequivalents per liter.2-3 Hypokalemia is a clinical sign of depressed potassium levels that is due to poor intake of potassium combined with other causes of hypokalemia.
What causes hypokalemia?
- Increased entry into cells due to:
-
- Increases in the activity of the Na-K-ATPase pump
- Increased availability of insulin
- Elevated beta-adrenergic activity
- Elevation in extracellular pH
- Hypokalemic periodic paralysis
- Increases in the activity of the Na-K-ATPase pump
- Increased blood cell production
- Hypothermia
- Intoxication with barium, cesium, and chloroquine
- Antipsychotic drugs
-
- Increased gastrointestinal losses
- Upper gastrointestinal loses –voluminous vomiting causes a rise in bicarbonate concentration due to large losses of gastric acid. This, in conjunction with hypovolemia- induced aldosterone secretion, causes increased potassium secretion and large urinary potassium losses.
- Lower gastrointestinal loses – mostly due to diarrhea.
- Increased urinary loses – potassium excretion occurs mostly in the distal nephrons and increased losses may be seen in diuretic use, increased aldosterone secretion, nonreabsorbable anions, and loss of gastric secretions.
- Increased sweat losses – for people exercising in very hot climates.
- Dialysis
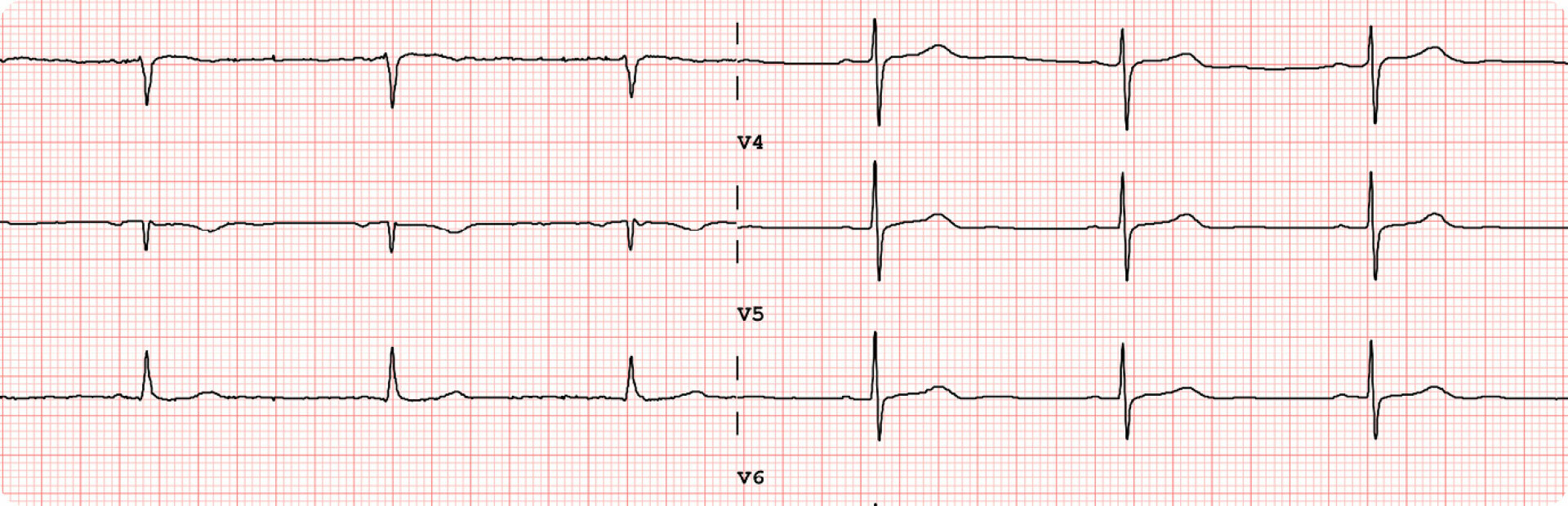
Symptoms of hypokalemia manifest when serum potassium levels fall below 3.0 milliequivalents per liter and these symptoms resolve once hypokalemia is corrected. These symptoms may include cardiac arrhythmias and electrocardiogram abnormalities such as ventricular tachycardia/ventricular fibrillation, paroxysmal atrial or junctional tachycardia, premature atrial and ventricular beats, sinus bradycardia, and atrioventricular block.4 Characteristic ECG changes in hypokalemia include ST segment depression, a decrease in T wave amplitude, and an increase in U wave amplitude. U waves are usually seen in the precordial leads of V4 to V6 (refer to Figure 1).

Figure 1. Hypokalemia ECG changes.
Other manifestations of hypokalemia include muscle weakness and rhabdomyolysis, as well as renal abnormalities: impaired concentrating ability, increased ammonia production, increased bicarbonate reabsorption, altered sodium reabsorption, hypokalemic nephropathy, and elevated blood pressure.5
What causes hyperkalemia?
Hyperkalemia results when there is impaired excretion of potassium due to acute or chronic kidney disease, or disorders or drugs that inhibit the rennin-angiotensin-aldosterone axis. It causes cardiac conduction abnormalities, cardiac arrhythmias, muscle weakness, and paralysis.6 These signs and symptoms manifest when the serum potassium concentration is greater than or equal to 7.0 milliequivalents per liter. Treatments involve inducing potassium loss.6-8
Electrocardiogram changes in hyperkalemia include a tall peaked T wave. As the degree of hyperkalemia becomes more severe, there is slowing of impulse conduction throughout the myocardium; the PR interval and QRS duration increases with a variety of conduction disturbances as follows:9
- Right bundle branch block, left bundle branch block, bifascicular block, and advanced atrioventricular block.
- Flattened P wave or no P wave secondary to atrial standstill or arrest.
- ST elevation in leads V1 and V2
- Widening of the QRS complex to a “sine wave” configuration.
However, there is no significant correlation between the progression and severity of ECG changes with the serum potassium concentration.
 Figure 2. ECG changes in hyperkalemia.
Figure 2. ECG changes in hyperkalemia.
Ascending muscle weakness is a manifestation of hyperkalemia that can progress to flaccid paralysis that is comparable to Guillain-Barre syndrome.10 Hyperkalemic periodic paralysis is an autosomal dominant mutation of sodium channels in skeletal muscles. Myopathic weakness develops in these patients after an increased intake of potassium or resting after vigorous exercise.
Careful monitoring of electrocardiogram changes and muscle weakness in hyperkalemia is important to determine its functional consequences. If these are observed to be severe, immediate correction of hyperkalemia is essential. If serum potassium increases rapidly, cardiotoxicity will ensue.
Sources:
- Rose BD, Post TW. Clinical Physiology of Acid-Base and Electrolyte Disorder, 5th ed, McGraw-Hill, New York, 2001, pp. 383-396, 898-910.
- Squires RD, Huth EJ. Experimental potassium depletion in normal human subjects. I. Relation of ionic intakes to the renal conservation of potassium. J Clin Invest 1959; 38:1134
- Gallen IW, Rosa RM, Esparaz DY, et al. On the mechanism of the effects of potassium restriction on blood pressure and renal sodium retention. Am J Kidney Dis 1998; 31:19.
- Rose BD, Post TW. Hypokalemia. In: Clinical physiology of acid-base and electrolyte disorders, 5th ed, Rose, BD, Post, TW (Eds), McGraw-Hill, 2001. p.836.
- Mujais SK, Katz, AL. Potassium deficiency. In: The Kidney: Physiology and Pathophysiology, Seldin DW, Giebisch G (Eds), Lippincott Wiliams & Wilkins, 2000. p. 1615.
- Mount DB, Zandi-Nejad, K. Disorders of Potassium Balance. In: Brener and Rector’s The Kidney, 8th ed, Brenner BM (Ed), W.B. Saunders Co, Philadelphia 2008. p. 547.
- Rose BD, Post TW. Clinical Physiology of Acid-Base and Electrolyte Disorder, 5th ed, McGraw-Hill, New York, 2001. p. 913.
- Kamel KS, Wei C. Controversial issues in the treatment of hyperkalemia. Nephrol Dial Transplant 2003; 18:2115.
- Bashour T, Hsu I, Gorfinkel HJ, et al. Atrioventricular and intraventricular conduction in hyperkalemia. Am J Cardiol 1975; 35:199.
- Evers S, Engelein A, Karsch V, Hund M. Secondary hyperkalemic paralysis. J Neurol Neurosurg Psychiatry 1998; 64:249.
Recommended Articles