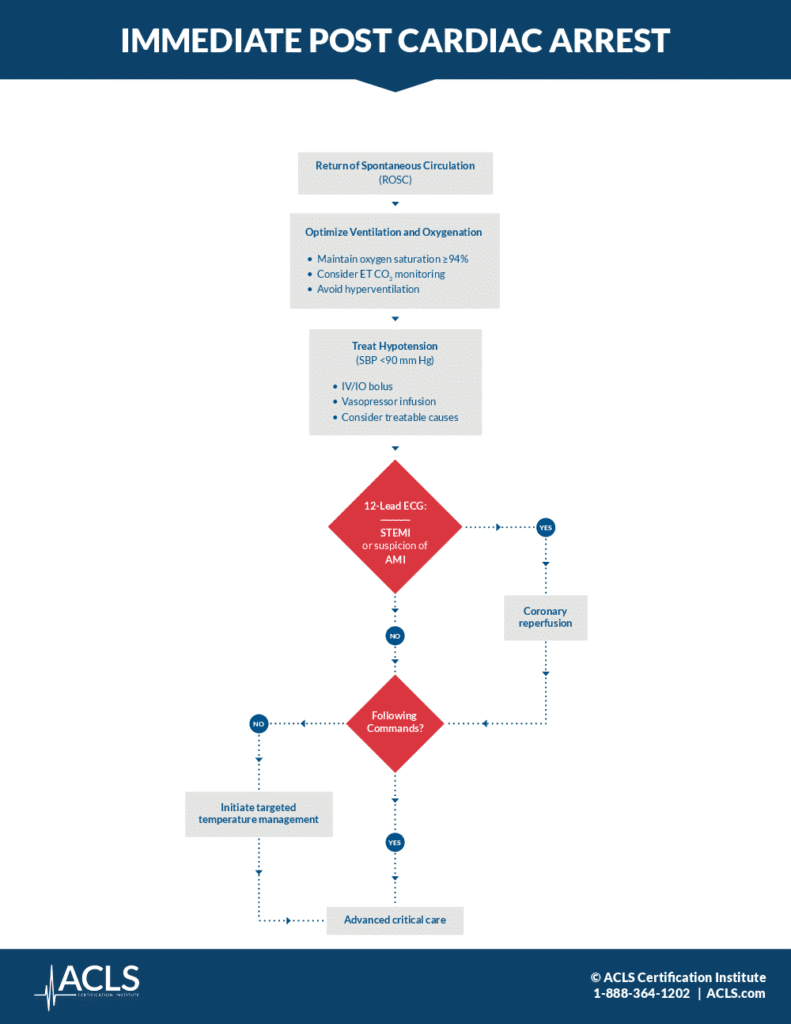
Immediate Post-Cardiac Arrest Care Algorithm

Learn more about post-cardia arrest treatment to improve patient outcomes with the ACLS post-cardiac arrest algorithm.
As with all ACLS algorithms, the Immediate Post-Cardiac Arrest Care Algorithm is a set of procedures that healthcare providers use to treat patients who have just experienced a specific medical emergency — in this case, cardiac arrest. Because cardiac arrest, or sudden, unexpected loss of heart function, breathing, and consciousness, is one of the most common medical emergencies, many nurses, EMS, physicians, and other healthcare providers will need to offer care for it at some point. That’s why preparation and training are critical. With the right care following the algorithm outlined below, successful resuscitation can often be achieved.
As part of our online ACLS course, you will learn the ins and outs of this set of the cardiac arrest algorithm and feel more confident knowing what to do when resuscitation is needed. For more information about the algorithm, including a description of each of its steps, keep reading.
-
- Achieve a return of spontaneous circulation (ROSC). Return of spontaneous circulation (ROSC) is the return of a detectable pulse and blood pressure. As the first step, this is a critical component of the resuscitation process because it indicates to you that the heart has resumed function and the vital organs are once again receiving oxygen. Immediate management of post-cardiac care after the return of spontaneous circulation can improve survival rates and functional recovery in the patient. You can achieve ROSC through several approaches, though the most common are CPR or defibrillation (both techniques you will learn more about in your ACLS online course).ROSC is critical, but there is much more involved in post-cardiac arrest treatment, That’s because patients who reach ROSC are at higher risk for complications such as brain injury, organ dysfunction, and sepsis. They require close monitoring and ongoing care, as outlined in the post-cardiac arrest algorithm, to improve their future outcome.
- Optimize ventilation and oxygenation. According to post-cardiac arrest guidelines, you should start with 10 breaths a minute, and use the lowest inspired oxygen concentration necessary to maintain SATs of 94% or greater. Use continuous waveform capnography to confirm and monitor the correct placement of the ET tube if needed. Avoid hyperventilation or the condition in which a person breathes faster or deeper than is necessary for the body’s oxygen demand. Hyperventilation can cause a severe drop in carbon dioxide (CO2) levels in the blood, a condition called respiratory alkalosis.
- Treat Hypotension (SBP <90 mm Hg). Check the patient’s blood pressure and treat for hypotension if needed. This is a condition where systolic blood pressure is less than 90. To do so, first, obtain IV access if it’s not already established, and verify the patency of the IV lines. Then treat the hypotension with IV bolus and vasopressor infusion. At this stage, consider treating any reversible causes that may have precipitated the cardiac arrest. These could include:
- Hypoxia – a lack of oxygen caused by airway obstruction, respiratory failure, or pulmonary embolism.
- Hypovolemia – a decrease in blood volume caused by external bleeding, dehydration, or other bodily fluid loss.
- Hypothermia – lowered body temperature caused by prolonged exposure to cold air or water.
- Hypokalemia or hyperkalemia – either low or high potassium levels in the blood.
- Presence of toxins – may be caused by drug overdose or toxic exposure.
- Cardiac tamponade – accumulation of fluid around the heart, which inhibits its pumping function.
- Thrombosis or pulmonary embolism – a blood clot that stops or reduces blood flow to the heart or lungs.
- Obtain a 12-Lead ECG: STEMI. Obtain a 12-lead ECG as soon as possible after the return of spontaneous circulation to identify patients with STEMI or a high suspicion of acute myocardial infarction (AMI).
- Begin coronary reperfusion. If STEMI is detected, EMS personnel should transport the patient to an appropriate facility quickly to reduce the time to treatment. Hospital personnel should begin coronary reperfusion with percutaneous coronary intervention (PCI).
- Check for an ability to follow commands. If STEMI or AMI are not detected, determine the patient’s ability to follow commands. Depending on if they are still comatose or awake, choose the following procedures.
- If comatose: Initiate targeted temperature management (TTM). If the patient is unable to follow commands or respond in a meaningful way, the high-performance team should initiate TTM.
- If awake: Transfer to advanced critical care. Once TTM has been initiated, or if the patient is responsive and able to follow commands, the patient should be transferred to advanced critical care as soon as possible to undergo further medical review and management.
Dive Deeper with Your ACLS Certification
ACLS algorithms just like these are key components of learning what to do in emergency, life-threatening situations. As part of our online ACLS course for healthcare providers, we break down this critical information into easy-to-learn steps that stick with you once the course is complete. Feel more confident in your Advanced Cardiovascular Life Support skills with the help of our flexible and affordable ACLS certification course.